Skin Grafts
A skin graft is a patch of skin that is surgically removed from one part of the body and transplanted to another. The skin graft replaces tissue that has been destroyed or creates new tissue where none exists. A skin graft can come from a different location on the same body or from a different person. The color and texture of the new graft is carefully chosen so that it fits the new site. Sometimes this is not possible, especially when a large area needs to be covered.
Skin Anatomy
The skin is composed of two layers. The thin epidermis layer is on top and the thicker dermis layer is underneath. Below the skin is the fatty subcutaneous tissue. Skin grafts are made from the epidermis and varying thickness of the dermis. Some grafts also include the subcutaneous tissue if it is to be used over bony areas or over tendons. This provides extra cushioning. Skin can regenerate at the donor site provided elements of dermis are preserved.
Types of Skin Grafts
The types of grafts are as follows:
- Split-thickness grafts, which contain the epidermis with only a portion of the dermis. These can be used over burns or large wounds. These may also be used where the conditions to support a skin graft are tenuous.
- Full-thickness grafts, which include all of the dermis. These types of grafts are best for covering small areas, where matching skin color and texture is important.
The use of Full Thickness Skin Grafts (FTSG) is contraindicated when the recipient bed, due to lack of reasonable vascular supply, cannot sustain the graft. Using an FTSG on avascular tissues, such as exposed bone or cartilage, most often leads to graft necrosis unless the area is small (and allows the bridging phenomenon to occur).
Uncontrolled bleeding in the recipient bed is another contraindication to the placement of an FTSG because hematoma and/or seroma formation under the graft compromises graft survival.
Who is a candidate for the procedure?
Skin is a protective barrier against infection and injury. When it becomes damaged and is no longer functional, a skin graft can be used to replace it. One of the most common uses of skin grafts is to replace badly burned tissue. Skin that has been destroyed due to trauma, such as a motor vehicle accident, can also be helped with skin grafts. Skin grafts may be used in reconstructing any part of the body after an injury, excisional surgery or for cosmetic reasons.
How is the procedure performed?
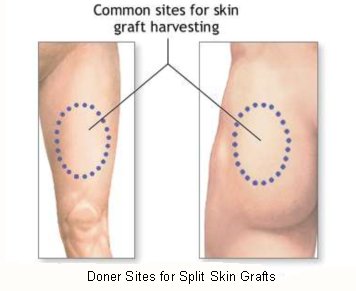
Skin grafting is performed by a surgeon in an operating room. Once the donor site is selected, the surgeon will remove a portion of skin big enough to fit the area it is to be transplanted to. This tissue or graft is removed and attached to the area in one procedure.
Sometimes the skin to be used as a graft can be stretched or grown over a period of time with special instruments inserted by a surgeon. In these cases, once the skin has reached the proper size it will be cut and transferred the recipient site.
The site to receive the graft must be clean and free from bleeding. If the area is dirty or infected, the surgeon will have to scrub it to remove any dead tissue or foreign material. Once the area is properly prepared the surgeon can attach the skin graft with sutures, staples or glue
Once the graft is in place it must be kept clean. The bleeding must be controlled. There shouldn't be any movement between the graft and its "bed." Sometimes the surgeon will make small holes in the graft to allow fluid to escape so it does not accumulate and disrupt the graft from the bed.
What happens right after the procedure?
Firm dressings over the graft will keep the graft from moving. It will also prevent fluid from accumulating. The dressing should be firm but still allow good blood flow. Also, the graft should be kept free of infection. The site must also be watched to make sure it is pink and healthy. This indicates good blood flow.
Before leaving the hospital, a person will be given special instructions on how to change the dressing as well as warning signs to look for that may indicate a problem.
What happens later at home?
The goal is to keep both the graft site and donor site clean and free from infection. The graft site is monitored for good circulation, as indicated by a healthy pink color. The donor site is also checked for signs of good healing without infection.
What are the potential complications after the procedure?
Complications following a skin graft include the following: · Infection can occur with the graft site or with the donor site. If the infection is too severe or proper blood flow is not maintained, the grafted skin can die.
Failure of the skin graft to survive at its new (recipient) site. This can be due a number of factors that include
- Haematoma (collection of blood) between the graft and the vascular bed
- Infection leading to graft loss
- Inadequate blood supply at the recipient site
- Persisting underlying disease (eg. Cancer)
- Sometimes the graft will pull away from the sides of the new site. This can cause a distorted shape or a feeling of tightness.
- Sensation to the graft site can also be affected. There may be an increase or a decrease in sensation.
- A new graft is also sensitive to sunlight and protective measures will always be necessary for the life of the graft.
Aftercare
The skin grafted site as well as the donor area have a tendency towards dryness, and require regular moisturising with the use of a cream (E 45, Diprobase, Nivea etc). Both areas are liable to sun damage and should be protected with a sun block when exposed to direct sunlight. The donor area often heals as a distinct hyper or hypo pigmented patch. Sometimes healing of the donor area may be complicated and delayed for a few weeks.
There are occasions when it appears that the skin graft has been lost. Most of the time there will be enough number of epithelial islands which will help the entire area epithelialise (ie. Get a covering of skin) with regular dressings.