Gynaecomastia (male breast development)
Gynecomastia is defined as the presence of an abnormal proliferation of breast tissue in males. It is a common breast lesion accounting for more than 65 percent of male breast disorders. Gynecomastia has a broad range of causes that are classified as either physiological or pathological, although in many cases no specific cause can be found. In true gynecomastia, the breast enlargement is due to glandular breast tissue; in pseudogynecomastia, the breast enlargement is secondary to fat accumulation; and both glandular and fat tissue are present in mixed gynecomastia.
What are the various types of Gynecomastia?
Physiologic gynecomastia occurs most frequently during times of male hormonal changes, resulting from the effect of an altered oestrogen/androgen balance on breast tissue or from the increased sensitivity of breast tissue to a normal oestrogen level.
Pubertal gynecomastia is a common condition with an overall incidence of 38 percent in males 10 to 16 years of age, increasing to 65 percent at age 14, and dropping to 14 percent in 16-year-old boys. During adolescence, 75 percent of the gynecomastia cases are bilateral but the breasts are often affected to different degrees. Pubertal gynecomastia often regresses spontaneously in six months, 75 percent within two years of onset, and 90 percent resolve within three years of onset.
Pathological gynecomastia is associated with both androgen deficiency and oestrogen excess. Both causes may be correlated to medications, diseases related to endocrinologic abnormalities, tumours, chronic disease, chromosomal abnormalities, familial disorders, and miscellaneous other conditions. While always a concern when a mass is present, breast cancer accounts for only 0.2 percent of all malignancies in male patients. A suspicious mass or lesion requires biopsy.
Causes include:
Drugs:
- medicinal:
- certain drugs for heart disease, ulcers, high blood pressure, chemotherapy agents
- recreational:
- Cannabis, heroin and methadone as well as anabolic steroids. Stopping the drugs will reduce any tenderness, but the breast tissue may persist.
Other causes:
- Liver disease
- Testicular tumours
- Testicles that are underdeveloped, or damaged through illness or trauma (eg following mumps)
- Tumours of the adrenal glands
- Altered thyroid function – usually overactive
- Kidney failure
- Obesity
Indications
The surgical treatment of gynecomastia has two objectives: reconstruction of the male chest contour, and histological clarification of suspicious breast lesions. The age of the patient, consistency, grade, and the presence of unilateral or bilateral breast development determine the indication for surgery. Prior to surgical consult, the gynecomastia patient should undergo a complete history and physical exam and appropriate diagnostic testing to determine the underlying cause of the gynecomastia.
Gynecomastia Scale adapted from the McKinney and Simon, Hoffman and Kohn scales:
| GRADE I | GRADE II | GRADE III | GRADE IV |
| Small breast enlargement with localized button of tissue that is concentrated around the areola. | Moderate breast enlargement exceeding areola boundaries with edges that are indistinct from the chest. | Moderate breast enlargement exceeding areola boundaries with edges that are distinct from the chest with skin redundancy present. | Marked breast enlargement with skin redundancy and feminization of the breast. |
Gynecomastia may cause considerable psychological distress, especially in adolescents who are struggling with issues related to sexual identity and self-image.
Prolonged presence of breast enlargement in the male patient leads to the development of periductal fibrosis and stromal hyalinisation, preventing regression of breast tissue and causing pain and discomfort due to the distension and tightness from the hypertrophied breast.
Procedures
The correction of gynecomastia involves removing the abnormal hypertrophic breast tissue and associated surrounding subcutaneous tissue so that the breast has a more normal male appearance. The specific surgical technique will vary depending on the degree of breast hypertrophy present and the amount of fat tissue versus breast tissue removed. A circumareolar incision to remove breast tissue may be adequate for a thin person with a small amount of hypertrophy. A reduction mammaplasty or subcutaneous mastectomy with skin reduction may be required for patients with larger hypertrophic breasts. There are times when a gynecomastia procedure will require a more extensive mastectomy. Suction assisted lipectomy may be used as the primary method of removing excess tissue or as an adjunctive procedure to contour the anterior chest wall.
Am I a good candidate for gynecomastia surgery?
You may be a good candidate for breast surgery if you have one or more of the following problems
- self-consciousness about the largeness of your breasts
- abnormal appearance not easily covered by clothing
- asymmetry in breast (chest) size
How will I be evaluated for breast reduction surgery?
Your plastic surgeon will examine your chest, taking measurements and perhaps photographs for your medical record. The size and shape of your breasts, the quality of your skin, and the placement of the nipples and areolas will be carefully evaluated.
You should come to the consultation prepared to discuss your medical history. This will include information about any medical conditions, drug allergies, medical treatments you have received, previous surgeries including breast biopsies, and medications that you currently take. It is important for you to provide complete information.
Liposuction
For a fair few corrective surgery is the best option. Unlike radical breast reduction in women, this is more like liposuction, with only a couple of small and inconspicuous incisions. The surgery is carried out under a general anaesthetic and takes about 90 minutes. General recovery time is about six weeks.
Liposuction is particularly well-suited for men who have an isolated pocket of fat. In case of existing excess skin a surgical approach is preferable.
Fat is removed by first inserting a small, hollow tube, called a cannula, through one or more tiny incisions near the area to be suctioned. Incisions are usually less than one-quarter inch in length and are placed as inconspicuously as possible, often within skin folds or contour lines. The cannula is connected by tubing to a vacuum pressure unit. Guided by the surgeon, the suction device literally vacuums away the unwanted fat.
Fortunately, significant complications from liposuction are infrequent. Every year, many thousands of people have their bodies re-contoured, experience no major problems and are pleased with the results. Anyone considering surgery, however, should be aware of both the benefits and risks.
Potential complications include bleeding, infection and reactions to anaesthesia. Blood accumulations under the skin are possible, but these normally resolve themselves and rarely require removal. While numbness of the skin following liposuction is almost always temporary, it is possible for some lack of sensation to persist or for skin discoloration to appear in treated areas. Contour irregularities including depressions or wrinkling of the skin can result in some patients, but treatments are usually available to help minimize these problems if they occur.
Excisional Surgery
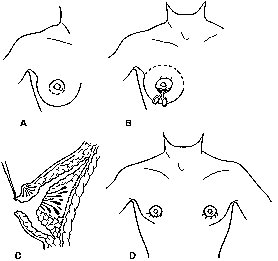
A circular incision is made at the junction of the skin and areola all around the circumference. In case of an existing skin excess, an area of skin would be excised as well. A disc of breast tissue is left beneath the areola to prevent the formation of a crater and to produce a smooth natural-looking chest. The skin is undermined, leaving a layer of fat beneath. The breast tissue and fatty disc are then dissected off the pectoral fascia and removed. The resulting cavity is drained with suction, as haematoma formation is common, and the wound closed. It is important to leave the nipple/areola complex in the correct position and symmetrical with the opposite side, with minimal obvious scarring.
Liposuction can be a useful adjunct, but only if the gynecomastia is mainly of the fatty variety. It can also be used to feather out the peripheral tissues to allow better contouring. Post-operatively, the breast should be dressed in such a fashion as to prevent ptosis developing in the undermined skin. This is done using an adhesive dressing to support the skin.
Understanding Risks
Fortunately, significant complications from gynecomastia surgery are infrequent. Every year, many men undergo successful breast reduction surgery, experience no major problems and are pleased with the results. Anyone considering surgery, however, should be aware of both the benefits and the risks
Potential Complications
- Scarring – visible, permanent, lumpiness
- Bleeding – need for drains which are removed once the drainage has decreased to approximately 25-30 mls/day. Potential for blood transfusion.
- Haematoma (blood collection)
- Seroma (collection of serum/altered blood). This may require aspiration with a large bore needle and invariable settles down with conservative management
- Altered sensation over the nipple areolar complex as well as the breast skin
- Asymmetry in size and shape
- Infection
- Lumpiness secondary to fat necrosis
- Necrosis or vascular impairment of the nipple
In case of failure with liposuction, excisional surgery may be required as a second stage